this photo of the news not showing the actual #mosjid ul #aksa.. (@masjidul aksa)
CREATION of ALLAH
some WORKS during MY free HOUR
এই ব্লগটি সন্ধান করুন
my self
- Md Sazzad Kader
- ibrahim medical college, dhaka, Bangladesh
- A follower of Mohammed (sm:)
বৃহস্পতিবার, জুন ৩০, ২০১১
পবিত্র শবে মিরাজ পালিত হচ্ছে <> sheershanews.com <> দেশের আরো খবর
পবিত্র শবে মিরাজ পালিত হচ্ছে <> sheershanews.com <> দেশের আরো খবর
রবিবার, জুন ১২, ২০১১
FeW discussion AbOuT : liver disease JaUnDiCe
Before discussion we should know some question to ask frequently..
what is liver?
-it is one of the largest organ of the body
where its location?
-most of its part located in right hypochondrium , extend to epigastrium
what are the parts of the liver?
-right lobe and left lobe.right lobe forms the three quarters of the liver
few anatomy of the liver ?
-macroscopic:
color : reddish brown
weight : about 1.5 kilogram
suspend on upper part of the abdomen through some
ligaments and peritoneal reflections :
a. right triangular ligament
b. left triangular ligament
c. falciform ligament
microscopic :
functional unit of liver : hepatic lobule
it is 1-2mm nodule around a tributary of central vein ,portal tract at
the peripheri.the portal tract contains a branch of hepatic artery , a branch
of portal vein and biliary duct
the main cell types are :
a. hepatocytes : - metabolically active
b. perisinusoidal (ITO) cells - synthesis of extra-cellular matrix glycoprotine(gp)collagen
c. others : kupffer cell(macrophage), stellate cells , lymphocyte
natural killer cells
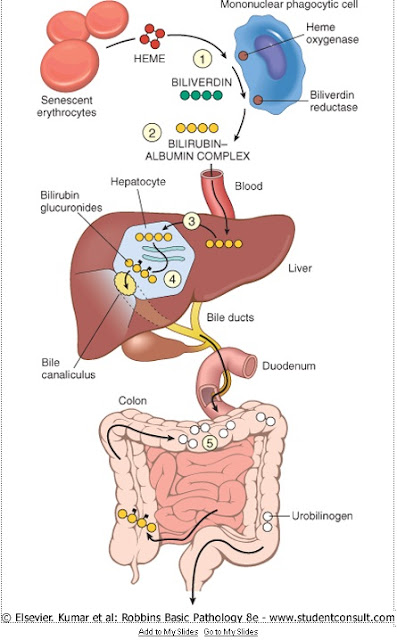
Unconjugated (indirect)
Erythrocytes (red blood cells) generated in the bone marrow are disposed of in the spleen when they get old or damaged. This releases hemoglobin, which is broken down to heme as the globin parts are turned into amino acids. The heme is then turned into unconjugated bilirubin in the reticuloendothelial cells of the spleen. This unconjugated bilirubin is not soluble in water. It is then bound to albumin and sent to the liver.
Conjugated (direct)
In the liver it is conjugated with glucuronic acid by the enzyme glucuronyltransferase, making it soluble in water. Much of it goes into the bile and thus out into the small intestine. Some of the conjugated bilirubin remains in the large intestine and is metabolised by colonic bacteria to urobilinogen, which is further metabolized to stercobilinogen, and finally oxidised to stercobilin. This stercobilin gives feces its brown color. Some of the urobilinogen is reabsorbed (enterohepatic circulation) and excreted in the urine along with an oxidized form, urobilin.
what is Jaundice?
Jaundice (also known as icterus;) is a yellowish pigmentation of the skin, the conjunctival membranes over the sclerae(whites of the eyes), and other mucous membranes caused by increased levels of bilirubin in the blood (hyperbilirubinemia )
broad classification of jaundice
-1. haemolytic
2. hepatocelluler
3. obstructive
pathophysiology of different types of jaundice :
The mechanisms responsible for jaundice:
1.include excess production,
2.decreased hepatic uptake or impaired conjugation of bilirubin,
3.intrahepatic cholestasis,
4.hepatocellular injury and
5.extrahepatic obstruction.
Jaundice becomes noticeable when the serum bilirubin level reaches approximately 3.0 mg per dL (52 (micro)mol per L).
UNCONJUGATED HYPERBILIRUBINEMIA
Unconjugated hyperbilirubinemia may result from excessive production of unconjugated bilirubin or from decreased ability to conjugate bilirubin.
Thus, the causes are:
a. hemolytic (excess production) or
b. hepatic (decreased conjugation).
Hemolysis may be due to
intrinsic defects in blood cells, such as
a. hemoglobinopathies,
b. enzyme abnormalities or
c. cell structure defects .
Extrinsic factors, including
a. drug toxicity,
b. infectious agents,
c. immunologic abnormalities,
d. malignancy and trauma, can also result in hemolysis.
Hepatic causes of unconjugated hyperbilirubinemia are:
1. disorders involving defective uptake and impaired conjugation of bilirubin.
2. decreased (UDP-glucuronyl transferase activity causes mild increases in unconjugated bilirubin eg. Gilbert's syndrome is a relatively common inherited condition
3. Physiologic jaundice of the newborn represents defective uptake due to immaturity of hepatic cells.
Breastmilk jaundice results from competitive inhibition of UDP-glucuronyl transferase by the maternal hormone pregnanediol.
Type 1 and type 2 nonhemolytic jaundice are manifestations of inherited defects that cause moderate or severe increases in unconjugated bilirubin. Type 1 nonhemolytic jaundice (formerly known as Crigler-Najjar syndrome) represents total absence of UDP-glucuronyl transferase and is usually fatal in infancy. Type 2 is characterized by a marked decrease in the enzyme.
CONJUGATED HYPERBILIRUBINEMIA
Conjugated hyperbilirubinemia occurs when bilirubin is returned to the bloodstream after conjugation in the liver, instead of draining into the bile ducts.
The most common causes are:
1. hepatocellular disease,
2. intrahepatic cholestasis and
3. extrahepatic obstruction.
Hepatocellular dysfunction: may be due to
a. hepatitis,
b. cirrhosis,
c. tumor invasion or
d. toxic injury .
Intrahepatic cholestatic syndromes: may occur in
a. hepatitis,
b. in pregnancy and
c. with certain medications, such as phenothiazines and estrogens.
The mechanism of drug-induced jaundice may be intrahepatic cholestasis or direct hepatocellular injury.
d. Primary biliary cirrhosis and cholangiocarcinoma also can induce cholestasis.
e. Dubin-Johnson and Rotor syndromes are rare inherited disorders that may cause
jaundice due to impaired excretion of conjugated bilirubin.
The most common causes are:
1. hepatocellular disease,
2. intrahepatic cholestasis and
3. extrahepatic obstruction.
Hepatocellular dysfunction: may be due to
a. hepatitis,
b. cirrhosis,
c. tumor invasion or
d. toxic injury .
Intrahepatic cholestatic syndromes: may occur in
a. hepatitis,
b. in pregnancy and
c. with certain medications, such as phenothiazines and estrogens.
The mechanism of drug-induced jaundice may be intrahepatic cholestasis or direct hepatocellular injury.
d. Primary biliary cirrhosis and cholangiocarcinoma also can induce cholestasis.
e. Dubin-Johnson and Rotor syndromes are rare inherited disorders that may cause
jaundice due to impaired excretion of conjugated bilirubin.
Extrahepatic obstruction:
occurs when :
a.stone,
b.stricture or
c.tumor blocks the flow of bile within the extrahepatic biliary tree.
occurs when :
a.stone,
b.stricture or
c.tumor blocks the flow of bile within the extrahepatic biliary tree.
Predominantly Unconjugated Hyperbilirubinemia c. Resorption of blood from internal hemorrhage (e.g.,alimentary tract bleeding,hematomas) I. Physiologic jaundice of the newborn |
Predominantly Conjugated Hyperbilirubinemia a. Deficiency in canalicular membrane transporters b. Drug-induced canalicular membrane dysfunction (e.g., oral contraceptives, cycloporine) c. Hepatocellular damage or toxicity (e.g., viral or drug-induced hepatitis, total parenteral nutrition, systemic infection) d. Impaired intra- or extra-hepatic bile flow e. Inflammatory destruction of intrahepatic bile ducts (e.g., primary biliary cirrhosis, primary sclerosing cholangitis, graft-versus-host disease, liver transplantation) |
laboratory diagnosis of jaundice (common for any liver diseases )
Test Category | Serum Measurement* |
Hepatocyte integrity Biliary excretory function Hepatocyte function | Cytosolic hepatocellular enzymes Substances secreted in bile Serum bilirubin Total: unconjugated plus conjugated Urine bilirubin Serum bile acids Plasma membrane enzymes(from damage to bile canaliculus) Serum alkaline phosphatase Proteins secreted into the blood |
শুক্রবার, নভেম্বর ২৬, ২০১০
সোমবার, সেপ্টেম্বর ২০, ২০১০
green leaf
from my tour at shreepur ..........some photo never get older ...... it just ever green ...........forever
এতে সদস্যতা:
মন্তব্যসমূহ (Atom)